(Vienna, 31 August 2024) In a study led by MedUni Vienna, previously unknown cellular processes in the occluded coronary artery that can lead to a heart attack have been revealed. At the same time, natural antibodies have been identified that can limit the damage caused by a heart attack. Despite medical advances, acute myocardial infarctions are still one of the most common causes of death in the western world. The study results published in the prestigious "European Heart Journal" provide a promising basis for the development of new, targeted therapies.
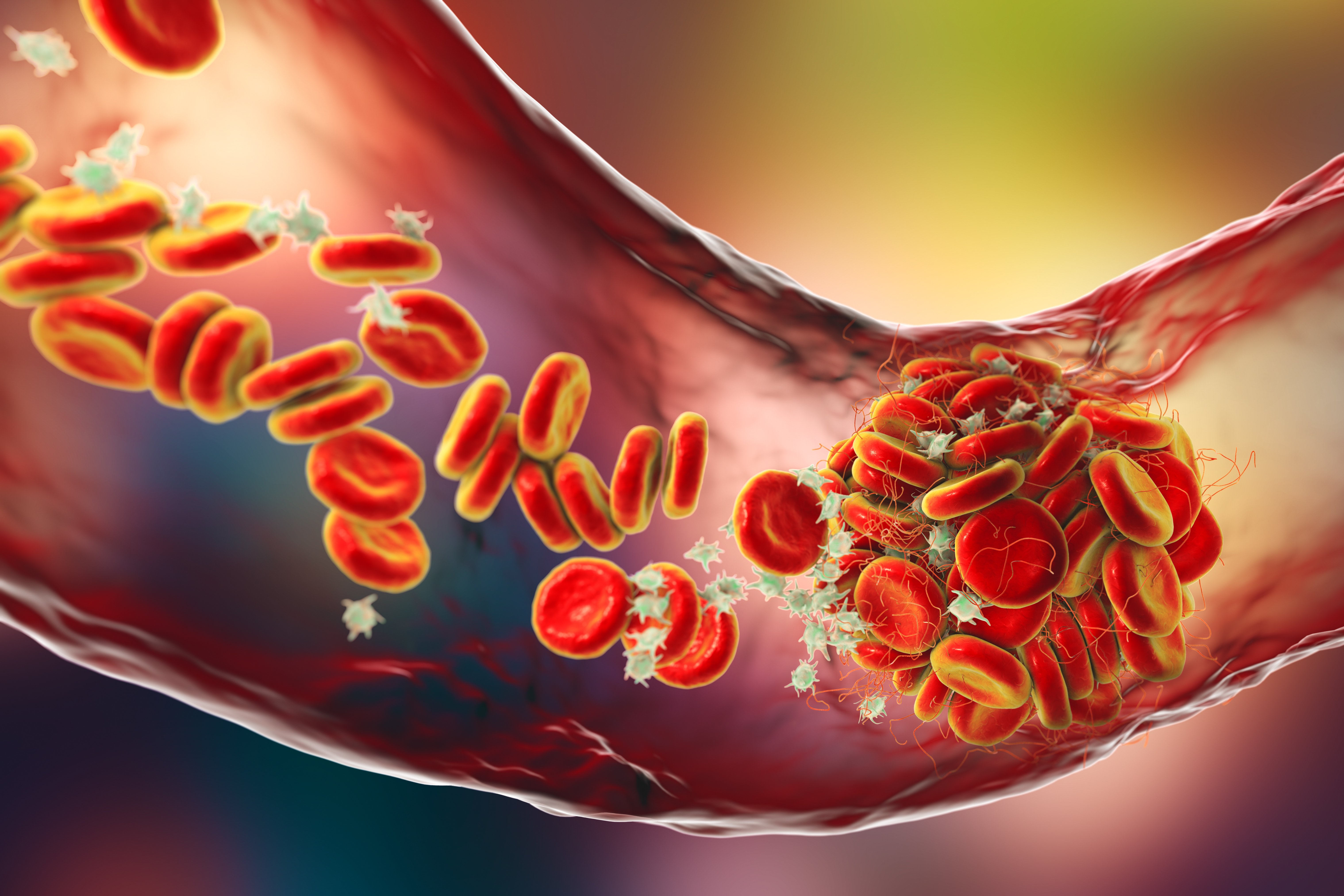
The new insights into the inflammatory process during the occlusion of a heart vessel were gained in a joint research project by Anna Ondracek and Taras Afonyushkin, two scientists from the interdisciplinary team of Christoph Binder (Department of Laboratory Medicine) and Irene Lang (Department of Medicine II, Clinical Division of Cardiology). The researchers built on established knowledge that many so-called extracellular vesicles are released from cells into the bloodstream at the time of a heart attack at the culprit lesions site in order to transmit signals between cells. In their current study, the research team was able to reveal important new details about the nature of these vesicles. For example, the analyses showed that the vesicles in the infarct vessel activate certain immune cells (neutrophil granulocytes), which can trigger the release of inflammation-promoting messenger substances and release so-called neutrophil extracellular traps (NETs). "The formation of NETs in the vascular system is critical because they can trap red blood cells and platelets, which can lead to thrombosis and blockage of coronary vessels and ultimately to a heart attack," explains co-first author Anna Ondracek.
Breaking the inflammatory cycle
According to the results, the process that has now been discovered promotes an inflammatory cycle that is associated with a deterioration in heart function. Against this background, the research team set out to identify the body's own protective factors that could break the vicious circle and came across innate antibodies of the IgM type. In various experiments, it was shown that the addition of specific IgM significantly reduces the release of NETs. In patients who had higher levels of these protective antibodies, a reduced production of NETs was also demonstrated. At the same time, high levels of these IgM antibodies meant better heart function after a heart attack. "Our data show that the increased production of pro-inflammatory factors can be compensated for by the presence of protective IgM," reports co-first author Taras Afonyushkin from the study.
According to the World Health Organisation (WHO), around 15 to 20 million people worldwide suffer an acute myocardial infarction every year, and around nine million die as a result. The infarction is triggered by the blockage of a coronary artery, which is caused by inflammation. This flares up at a specific region in the blood vessel and forms a blood clot (thrombus) within seconds. The exact mechanisms of vascular occlusion are still not fully understood. "In our study, we were not only able to identify the factors that trigger vascular occlusion via NETs and thus a heart attack, but also the mechanisms that can protect against damage," say study leaders Christoph Binder and Irene Lang, summarising the significance of the results, which represent a promising basis for the development of targeted therapies.
Publication: European Heart Journal 2024
Malondialdehyde-specific natural IgM inhibit NETosis triggered by culprit site-derived extracellular vesicles from myocardial infarction patients.
Anna S. Ondracek▲, Taras Afonyushkin▲, Adrienne Aszlan, Soreen Taqi, Thomas Koller, Tyler Artner, Florentina Porsch, Ulrike Resch, Smriti Sharma, Thomas Scherz, Andreas Spittler, Maximilian Haertinger, Thomas M. Hofbauer, Maria Ozsvar-Kozma, Veronika Seidl, Dietrich Beitzke, Marcus Krueger, Christoph Testori, Irene M. Lang*, Christoph J. Binder*
DOI: 10.1093/eurheartj/ehae584