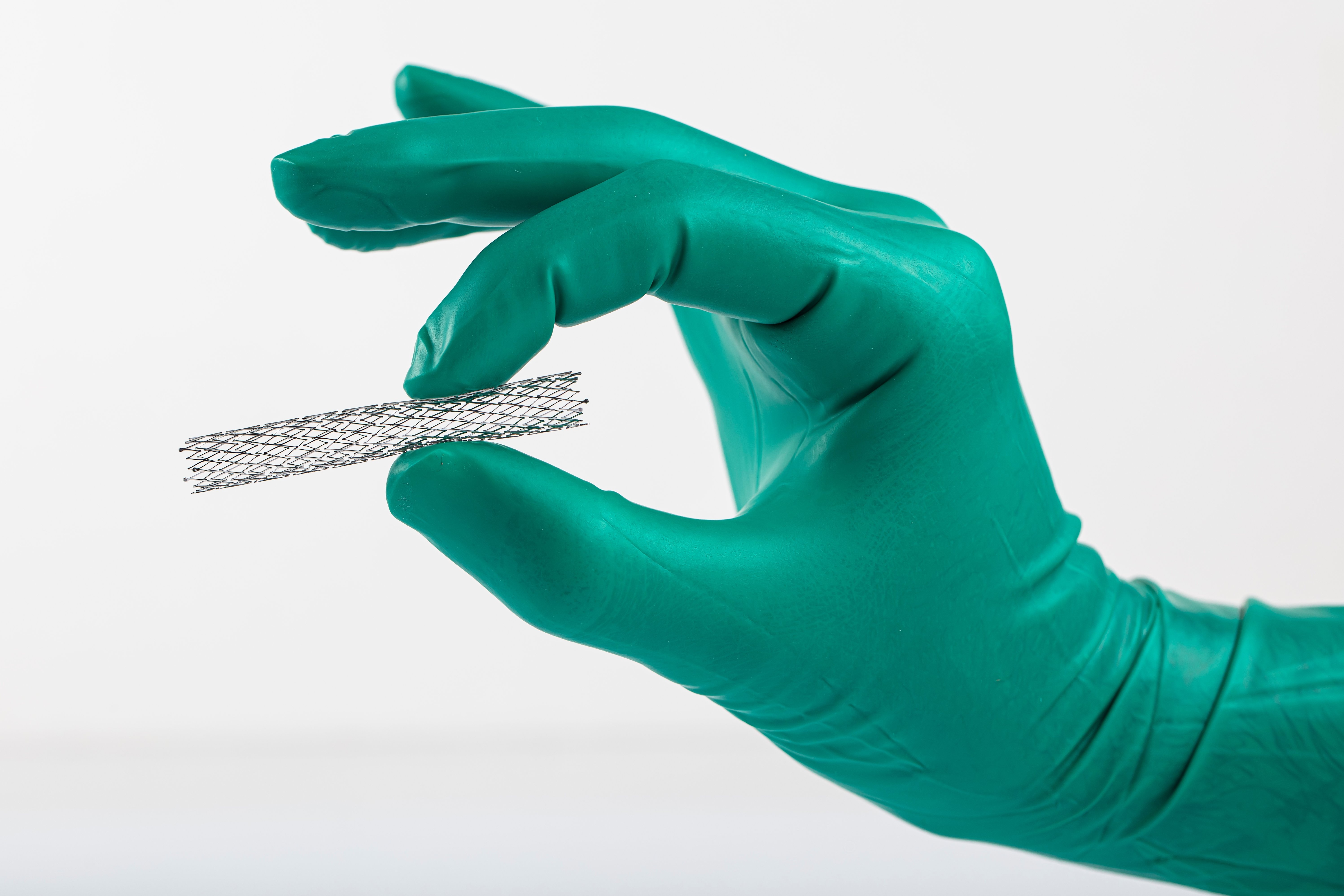
(Vienna, 29-01-2024) Coronary stents are implanted in more than 26,000 patients in Austria every year to treat angina pectoris or heart attacks. These are vascular stents made of metal that help to keep narrowed vessels open for many years. Acute clot formation (thrombosis) is the most feared complication of these procedures. A study recently published by MedUni Vienna in the Journal of the American Heart Association (JAHA) has now shown for the first time that acute inflammation increases the risk of stent thrombosis threefold.
As part of the study, the team led by first author Konstantin Krychtiuk and principal investigator Walter Speidl (Division of Cardiology at MedUni Vienna's Department of Medicine II) analysed data from 11,327 patients who had received a stent over the past decade. This measure was indicated due to atherosclerotic deposits in the coronary arteries, which had led to narrowing and thus to angina pectoris or heart attacks. In addition to bypass surgery, the most common treatment method in such cases is the implantation of coronary stents as part of a cardiac catheterisation. Despite major medical advances, 0.8 to two per cent of patients still experience potentially life-threatening stent thrombosis, i.e. acute blockage of the implant by blood clots, within 30 days. According to the main result of the analysis, the risk of this complication triples if there is acute inflammation at the time of the cardiac catheterisation. This was determined by increased levels of the inflammatory marker C-reactive protein (CRP) and the number of white blood cells. Blood tests are routinely carried out in preparation for a cardiac catheterisation.
Pneumonia particularly risky
As the scientific studies showed in detail, the rate of stent thrombosis in patients with low inflammation values was relatively low at 0.6 to 1.1 per cent. However, if CRP values of more than 50 mg/l or a leucocyte count of more than 12 G/l were present, the rate increased almost threefold to 2.1 to 2.8 per cent. Pneumonia and septicaemia in particular were frequently associated with stent thrombosis. "It is therefore important that only urgently needed stents are implanted in cases of acute inflammation, for example in the context of an acute myocardial infarction. Otherwise, the procedure should be postponed until the infection has subsided," Konstantin Krychtiuk and Walter Speidl summarise the essence of the results. The next step will be to confirm the findings in multi-centre studies before clinical guidelines are adapted accordingly.
In Austria, more than 26,000 coronary stents are implanted every year to treat angina pectoris or acute myocardial infarction. "In recent years, the incidence of stent thrombosis has been significantly reduced thanks to modern stents, improved implantation techniques and very potent drugs to inhibit platelets," reports study author Christian Hengstenberg, Head of the Division of Cardiology at MedUni Vienna's Department of Medicine II, from research and clinical practice. The fact that this complication, which is fatal in 20 per cent of cases, still occurs is mainly attributed to the premature discontinuation of antiplatelet drugs.
Publication: Journal of the American Heart Association (JAHA)
Association of Periprocedural Inflammatory Activation With Increased Risk for Early Coronary Stent Thrombosis;
Konstantin A Krychtiuk, Konstantin Bräu, Stephanie Schauer, Alexander Sator, Lukas Galli, Andreas Baierl, Christian Hengstenberg, Clemens Gangl, Irene M Lang, Christian Roth, Rudolf Berger, Walter S. Speidl;
Doi: 10.1161/JAHA.122.032300