Definition
Pulmonary hypertension (PH) is present when there is increased blood pressure in the pulmonary circulation. In children, as in adults, PH is defined by a pulmonary artery mean pressure ≥ 25 mm Hg at rest. This definition requires an invasive measurement during cardiac catheterisation. The method commonly used in everyday life to estimate the pressure in the lungs is echocardiography. If tricuspid regurgitation is present, the systolic pressure in the lungs can be estimated. If the measured systolic pressure in the lungs is equal to or more than 2/3 of the systemic pressure, pulmonary hypertension can be assumed.
Occurrence and pathogenesis
PH occurs in a variety of diseases, the different forms are categorised according to the currently valid Dana Point classification. This classification is only partially applicable to paediatric PH, as different entities of the Dana Point classifivation often occur simultaneously in childhood; the consensus paper founded in Panama in 2011 takes into account the diversity and peculiarities of paediatric PH in the classification.
Despite the diversity of PH forms, three main factors appear to be responsible for the increased resistance in the pulmonary circulation: vasoconstriction (vascular constriction), remodelling of the pulmonary vascular wall and thrombosis (clot formation) in situ.
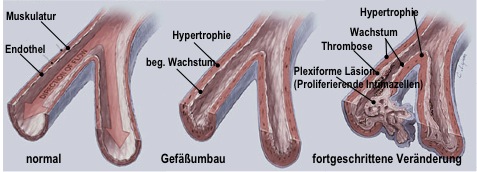
The decisive pathogenetic factor here is endothelial dysfunction, which can develop via various noxious agents such as hypoxia, mechanical lesions (shear stress), inflammation or against the background of a genetic disposition, but also via as yet unexplained mechanisms. This results in a disruption of the normal balance between vasodilators (vasodilating substances) and vasoconstrictors (vasoconstricting substances), between growth inhibitors and mitogenic factors and between antithrombotic and prothrombotic determinants. Histologically, this results in a uniform picture of obliterative vascular remodelling of the pulmonary arteries. Concentric intimal thickening, hypertrophy of the media, as well as fibroblast proliferation of the adventitia, thrombi in the small pulmonary vessels, and finally so-called "plexiform lesions" - small glomerular-like vascular balls - represent a pattern that is present in all PH forms to a greater or lesser extent. (see Fig. 1)
Clinic and diagnostics
Similar to adults, shortness of breath during physical exertion is a very early symptom in childhood. However, this is non-specific and is often interpreted as a lack of physical fitness or bronchial asthma. More advanced symptoms are chest pain, reduced exercise tolerance, dizziness and syncope. The latter are the result of the limited ability to increase cardiac output and thus also the oxygen supply to the organs under stress. It is not uncommon for children with syncope to be misdiagnosed as having a cerebral seizure disorder.
Delayed diagnosis with a latency of currently 2 years on average is therefore not uncommon. However, awareness of this disease has increased in recent years. Despite the unspecific symptoms, a thorough physical examination with a detailed family history can be the basis for a suspected diagnosis.
It is interesting to note that in children, in contrast to adults, there is a clear discrepancy between the pulmonary artery pressure values determined and the clinical symptoms. At the time of diagnosis, children usually have significantly higher pressure values in the small circulation than adults.
The following examinations are recommended by national and international associations to confirm the diagnosis: 12-lead ECG, lung X-ray, transthoracic echocardiography and cardiac catheterisation. The differential diagnosis of the various causes requires a lung function test, an arterial blood gas analysis with subsequent pulse oximetric oxygen saturation over 24 hours, possibly a sleep laboratory examination and a ventilation/perfusion scintigraphy.
Depending on the constellation of findings, various highly specialised examination methods (e.g. cardiac MRI, HRCT, multislice CT, pulmonary angiography) may be used for further clarification.
In addition to the exact classification of PH, the aim of diagnostics is also to determine the severity of the disease with NYHA classification, which is difficult in children.
Spiroergometry and the 6-minute walk test are used to assess exercise capacity; the latter is possible from around the age of 4.
Among the diagnostic examination procedures, cardiac catheterisation plays a decisive role. In addition to the exact determination of pressure and resistance ratios, it allows the responsiveness of the pulmonary vascular bed to be tested. On the one hand, the measurement results are used to determine the drug therapy. On the other hand, they can be used to decide on operability in children with PH due to heart defects. In children with severe non-operable heart disease, the measurement results are used to decide whether a heart transplant is possible.
In larger children, cardiac catheterisation can be performed under local anaesthesia without sedation; in smaller or uncooperative children, it is performed under analgosedation.
Therapy
Supportive measures:
All therapeutic measures are aimed at avoiding additional vasoconstriction due to hypoxia (drop in oxygen) or hypercapnia (increase in carbon dioxide) and achieving improved pulmonary blood flow.
Supportive therapies are all measures other than specific vasodilators, i.e. oral anticoagulation, glycosides, diuretics, but also physical rest and oxygen administration at saturations below 93%-90%.
As a reduced alveolar oxygen concentration leads to additional pulmonary vasoconstriction, corresponding situations such as stays at high altitude or air travel should be avoided or only carried out with a continuous supply of oxygen (e.g. O2 mask when flying).
In general, a pneumococcal, RSV and influenza vaccination is recommended for children with PH, including environmental prophylaxis for family members.
Pulmonary infections should be treated generously, possibly under inpatient conditions and with additional oxygen administration, including consistent fever reduction and possibly rehydration, as metabolic acidosis can exacerbate pulmonary hypertension due to the increased metabolism during fever.
Acute fluid loss, such as in the case of severe gastroenteritis, must be consistently compensated for, as the preload-dependent right ventricle can otherwise react with an acute drop in cardiac output.
Girls and young women should be informed about adequate contraception, as pregnancy and childbirth are associated with a high risk (mortality 30-50%).
Vasoactive therapy
The treatment concept is based on the increasing understanding that PH is the result of progressive vascular disease, which leads to increasing vascular obstruction through proliferation (growth), inflammation (inflammation) and vasoconstriction (vasoconstriction). The treatment algorithms aim to influence these components of vascular obstruction.
The substances used inhibit vasoconstriction through pharmacological vasodilation and slow down the structural vascular remodelling processes through anti-inflammatory and anti-proliferative effects ("anti remodelling strategy").
Calcium channel blockers
This very heterogeneous group of substances prevents the influx of calcium through the slow calcium channels of heart and smooth muscle cells, resulting in vasodilation of the pulmonary vessels.
Calcium channel blockers are given to patients with responder status, i.e. patients whose vascular reactivity is preserved during the cardiac catheterisation.
In the long term, only about half of haemodynamic responder children benefit from high-dose calcium antagonists as monotherapy. Therefore, strict therapy monitoring with regular re-evaluation of vascular reactivity during cardiac catheterisation is required.
Prostacyclins

Vasodilation is mediated by the activation of specific PGI2 membrane receptors that are coupled to the adenylate and guanylate cyclase system. Other effects, also mediated by specific receptors, include the inhibition of platelet activation and aggregation, but also the adhesion of leukocytes to endothelial cells. The introduction of prostacyclin therapy in the 1980s significantly improved the survival of PH patients.
Prostacyclin has a half-life of 3 minutes and must therefore be administered parenterally, i.e. intravenously. To ensure a continuous and safe supply, a central venous vascular access must be established and the substance (Flolan® ) is infused via a pump which the patient carries in a rucksack (see illustration). Due to the instability of the substance, the medication is freshly prepared every day. This form of therapy is very complex and associated with a high risk (catheter infection, thrombosis) and therefore requires detailed counselling, training and support for patients and parents of affected children.
The prostacyclin derivative iloprost (Ilomedin®) is more stable with regard to light and temperature sensitivity and has a longer half-life of 30 minutes. Compared to Flolan® and it therefore offers advantages in intravenous handling.
Iloprost (Ventavis®) can also be used inhaled; due to its duration of action, around 6-12 inhalations per day are necessary.
Treprostinil (Remodulin®), another prostacyclin analogue, can be administered intravenously or subcutaneously; due to the side effects (local pain, swelling), this form of administration has not proved successful in children.
Bosentan
Bosentan (Tracleer®) is the first dual endothelin receptor antagonist (ERA) approved on the market for the oral treatment of PH. Endothelin is increasingly produced in PH and promotes vasoconstriction and remodelling of the pulmonary vessels by binding to endothelin receptors (ET-A and ET-B receptors). By blocking the ET-A and ET-B receptors, bosentan combines vasodilatory with anti-inflammatory and anti-fibrotic effects.
According to the guidelines, bosentan is indicated for PH with non-responder status (without preserved vascular responsiveness). The efficacy of this drug has now also been well studied in children. Bosentan is well tolerated and safe and is taken twice daily. However, regular monitoring of liver parameters is recommended due to the side effect profile.
Ambrisentan is a selective endothelin A receptor antagonist and is currently only authorised for adults in Europe.
Sildenafil
Sildenafil (Revatio®) is a phosphodiesterase inhibitor and inhibits the breakdown of cyclic guanosine monophosphate (cGMP), which is increasingly released intracellularly by endogenous NO and leads to vasodilation. Sildenafil thus enhances the NO effect and also has antiproliferative effects. It has a firm place in the treatment of PH and has also been authorised for children with PH in Austria since 2011. Sildenafil is used for non-responder status and is generally well tolerated. Sildenafil is administered 3-4 times a day, occasionally in very special cases - more frequent administration is also necessary.
In children, flushing (flushing), headaches and a drop in blood pressure may occasionally occur at the beginning, but these side effects are dose-dependent and can usually be largely avoided by carefully tapering the drug.
Tadalafil, a longer-acting phosphodieesterase inhibitor, is currently only authorised for use in adults.
Combination therapies and other measures
The above-mentioned therapies are used individually according to the form of PH, the severity of the disease and the haemodynamically determined values.
As these therapies work via different mechanisms, the combination of these preparations makes sense and has also proven itself in everyday clinical practice, as this simultaneously attacks various mechanisms that initiate and drive vascular remodelling.
In the case of increasing right heart failure or the occurrence of syncope, an atrioseptectomy can be helpful. A cardiac catheter is used to create a small atrial septal defect, creating a kind of "pressure relief valve" at the atrial level. The presence of such a small interatrial communication has a preventive character with regard to acute right heart failure or a "low cardiac output" syndrome, albeit with the acceptance of undersaturation through the R/L shunt.
Outlook and summary
With increasing research into the complex mechanisms involved in the development of this vascular disease, further targets and thus therapeutic approaches in line with the anti remodelling strategy have been discovered in recent years, including Rho kinase inhibitors or tyrosine kinase inhibitors such as imatinib (Gleevec®), both of which are currently undergoing clinical trials.
The understanding of this disease and the use of the new drugs have opened up completely new perspectives for children with PH. Both quality of life and prognosis have improved significantly over the last two decades.
Nevertheless, PH remains a progressive disease that leads to right heart failure. In most cases, despite medical advances, no real cure can be achieved, only a slowing of its progression.
After all medical and interventional measures have been exhausted, lung or heart-lung transplantation is the last therapeutic option. Here too, the chances of survival have improved in recent years thanks to technical developments and new therapeutic approaches.
Updated clinical classification of pulmonary hypertension according to Dana Point 2008
The screening card for pulmonary hypertension can be found HERE