(Vienna, 10 December 2020) Patients with myeloproliferative neoplasm (MPN), a group of malignant diseases of the bone marrow, often have a carcinogenic mutated form of the calreticulin gene (CALR). Scientists of the research group of Robert Kralovics, Adjunct Principal Investigator at the CeMM Research Center for Molecular Medicine of the Austrian Academy of Sciences and research group leader at MedUni Vienna, have now identified hematoxylin as a novel CALR inhibitor. The study, published in the renowned journal Blood, shows how hematoxylin compounds affect a specific domain of CALR and selectively kill those CALR mutant cells that have been identified as the cause of disease in MPN patients. The discovery has enormous therapeutic potential and gives hope for new treatment options.
In medicine, a group of malignant diseases of the bone marrow is known as myeloproliferative neoplasms. This special type of blood cancer is characterised by increased formation of blood cells, vulnerability to thrombosis and frequent transformation to acute leukaemia. In the laboratory of Robert Kralovics it was discovered as early as 2013 that carcinogenic mutations of the gene calreticulin (CALR) were frequently found in affected patients and are now used clinically as diagnostic and prognostic markers. The mechanism by which the mutated CALR functions as an oncogene, which can lead to myeloid leukaemia, has also been scientifically identified since then. The carcinogenic effect of CALR mutations is based on the interaction of the N-glycan binding domain (GBD) of CALR with the thrombopoietin receptor. Ruochen Jia from the research group of Robert Kralovics at CeMM was looking for a way to stop this interaction and prevent one of the growth advantages of CALR mutated cells. It became evident that a group of chemicals, most notably hematoxylin, can selectively kill mutated CALR cells. The results thus provide extremely valuable information for potential treatment approaches for myeloproliferative neoplasms.
Hematoxylin compounds kill CALR mutated cells
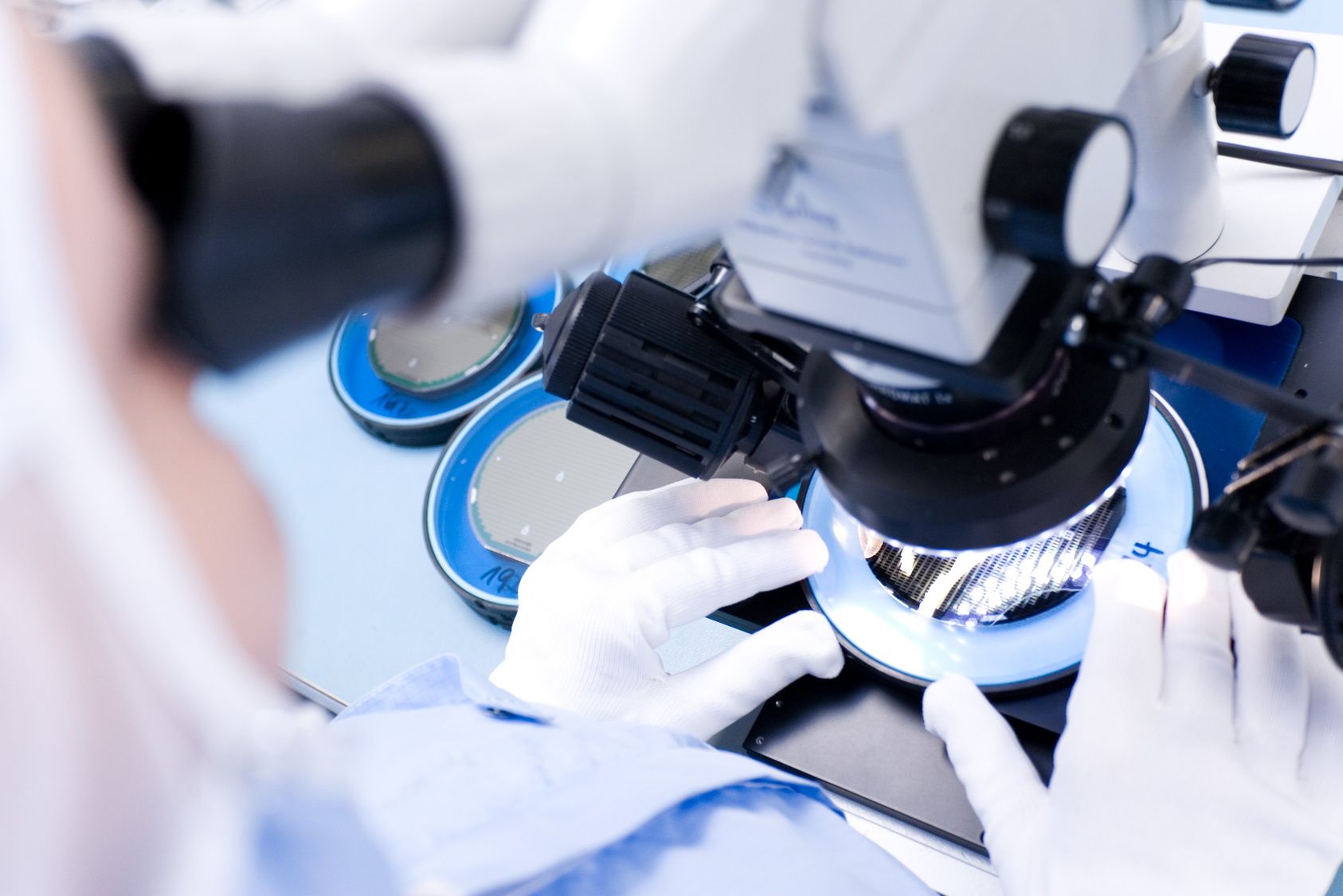
Robert Kralovics, head of the study, explains: “In our study we tried to identify small molecules that might block the interaction between the mutated CALR and the receptor.” The scientists used so-called in-silico docking studies for this purpose. “Basically, these are computer-based simulations of biochemical processes – virtual ‘screenings’ that enable increasingly accurate predictions,” says study first author Ruochen Jia. The results showed a group of chemicals as binders for a specific domain of calreticulin, which selectively kill the mutated CALR cells. “Our data suggest that small molecules targeting the N-glycan binding domain of CALR can selectively kill CALR-mutated cells by disrupting the interaction between CALR and the thrombopoietin receptor and inhibiting oncogenic signal transmission,” said the study authors. A hematoxylin compound proved to be particularly efficient. So far, hematoxylin has been used as a dye especially in histological staining processes.
Ray of hope for primary myelofibrosis therapy
“Our study demonstrates the enormous therapeutic potential of CALR inhibitor therapy,” says Kralovics. “The treatment of patients with primary myelofibrosis (PMF) continues to produce poor clinical outcomes. They have the clearest tendency to develop acute myeloid leukaemia. Since about one third of PMF patients have a CALR mutation, they could particularly benefit from the new therapeutic approach.”
Service: Blood
„Hematoxylin binds to mutant calreticulin and disrupts its abnormal interaction with thrombopoietin receptor“
Ruochen Jia, Thomas Balligand, Vasyl Atamanyuk, Harini Nivarthi, Erica Xu, Leon Kutzner, Jakob Weinzierl, Audrey Nedelec, Stefan Kubicek, Roman Lesyk, Oleh Zagrijtschuk, Stefan N Constantinescu, Robert Kralovics; published in "Blood".
DOI: https://doi.org/10.1182/blood.2020006264.
This study was supported by the Austrian Science Fund FWF (FWF SFB F4702, P29018-B30, FWF Stand-Alone P 30041-B26).