Aortic coarctation (CoA)
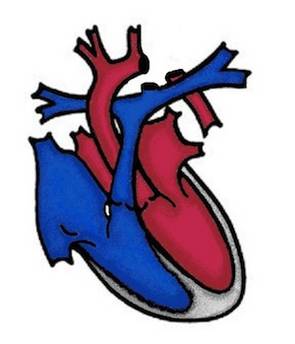
Aortic coarctation (coarctatio aortae) is a narrowing of the main body artery (aorta) shortly after the arteries branch off to the upper half of the body. This region is called the aortic isthmus and gives the disease its name. The aortic isthmus is the region where the patent ducuts arteriosus (PDA) joins. This malformation is also a heart defect, although it is actually a vascular malformation. It occurs both in isolation and together with a bicuspid aortic valve.
What are the effects of aortic coarctation?
In the left ventricle, which pumps the oxygen-rich blood into the ascending aorta and further into the aortic arch, the narrowing in the aortic isthmus results in increased blood pressure. This is passed on to all vessels that branch off from the aortic arch before the constriction, so that high blood pressure is created in the upper half of the body and low blood pressure is measured after the constriction.
Symptoms
Children with only a slight narrowing may be symptom-free.
Newborns with severe narrowing are seriously ill as soon as the ductus arteriosus closes in the first few days after birth. They may have difficulty drinking, shortness of breath, reduced kidney function and life-threatening circulatory problems. If the diagnosis is not made quickly, the child may die from cardiovascular failure.
In older children, the diagnosis is made by the appearance of a heart murmur. Sometimes, however, it is also the effects of high blood pressure in the upper half of the body, such as headaches, visual disturbances, behavioral problems with restlessness and hyperactivity, that lead to the diagnosis.
How is aortic coarctation treated?
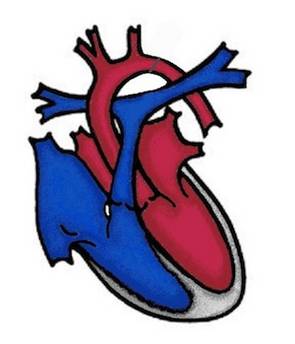
Emergency treatment: If the newborn's circulation is so restricted by the narrowing of the aorta that the situation is life-threatening, the ductus arteriosus can be kept open with a drug (prostaglandin) to ensure blood flow to the lower half of the body. In individual cases, balloon dilatation can be a life-saving emergency procedure.
Operation:
If the aortic isthmus is effectively narrowed, the narrowed part of the aorta is surgically removed and the remaining ends are sutured together (end-to-end anastomosis). In newborns, the ductus arteriosus is also closed at the same time. In addition to the end-to-end anastomosis, the most commonly used procedure today, it may be necessary to widen the aorta (e.g. subclavian flap operation). This is always necessary if the constriction is somewhat longer. In the case of surgery in infancy/toddlerhood, scarring can lead to a new narrowing as the patient grows.
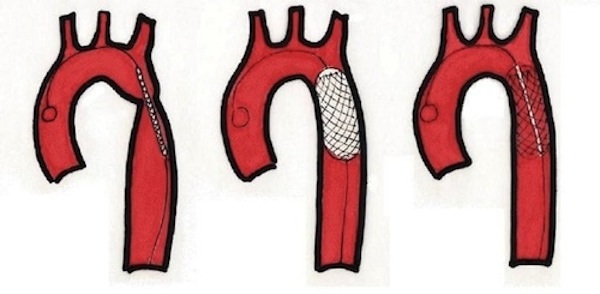
Cardiac catheter intervention
In older children and adolescents, it is also possible to perform a balloon dilatation of the aortic coarctation without heart surgery as part of a cardiac catheterization procedure. This technique is used as a standard therapy if a narrowing occurs again in the area of the suture after an operation. In patients where balloon dilatation alone is not sufficient or where there is a weakness in the wall of the aorta, the "diseased" aortic isthmus can be kept open permanently with a vascular support (stent implantation).
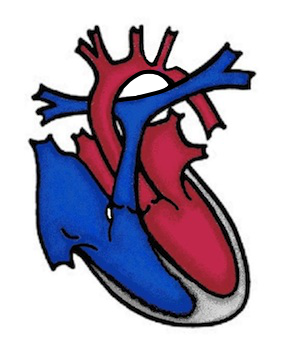
Controls
Even after a successful operation or cardiac catheter intervention, it is not uncommon - especially in older children - for blood pressure to remain elevated for some time and for antihypertensive medication to be taken.High blood pressure is a serious condition and must be carefully monitored and managed. Depending on the findings, the check-ups in the cardiac outpatient clinic are supplemented by special examinations such as a 24-hou blood pressure measurement or a stress ECG stress ECG. If the aortic isthmus in older patients can no longer be adequately assessed using Hcardiac ultrasound (echocardiography), magnetic resonance imaging (MRI) will provide clarity about the post-operative/post-interventional findings.