In a hypoplastic right heart, parts of the right side of the heart are underdeveloped in different ways.
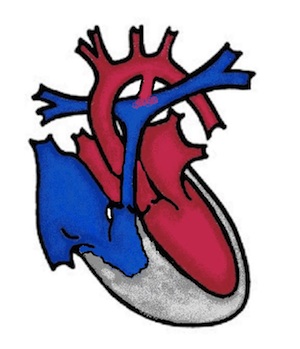
These include the tricuspid valve (heart valve between the right atrium and right ventricle), the right ventricle (right main chamber), the pulmonary valve (heart valve of the pulmonary artery) and the pulmonary arteries (pulmonary arteries). The heart valves can be narrowed (stenotic) or completely closed (atretic). Tricuspid atresia link and pulmonary atresia link therefore also belong to this clinical picture. As the right side of the heart is not functional, the baby relies solely on the left side of the heart for blood flow to the body and lungs.
What are the effects of hypoplastic right heart syndrome?
While the baby is usually quite well in the womb, cyanosis develops after birth as not enough blood can be pumped into the lungs. In order for the baby to survive, blood must be supplied to the lungs from the aorta via the ductus arteriosus (vessel between the pulmonary artery and the aorta). However, the ductus arteriosus usually closes in the first hours to days after birth and the drug prostaglandin must be administered quickly to reopen the ductus arteriosus. In addition, the child needs an open foramen ovale, so that the deoxygenated blood from the body can mix with the blood from the left side of the heart. If this connection between the right and left atrium of the heart is too small, it can be widened with a cardiac catheter intervention (Rashkindprocedure).
Symptoms
Children with HRHS are cyanotic (blue), breathing is often laboured and sometimes fluid accumulates in the body (oedema).
How is hypoplastic right heart syndrome treated?
A child with HRHS has the best prospects if the diagnosis is known before birth. The delivery is then planned in a centre that has experience in the care of these children, so that the medication prostaglandin can be started as a continuous infusion immediately after birth.
Operation
In HRHS there is also no way to stimulate the underdeveloped right side of the heart to grow. The surgical options depend on whether all sections of the right heart are underdeveloped or only individual parts are affected. In tricuspid atresia, the right ventricle is so small that the left side of the heart has to take over the entire work of the heart in the long term. In pulmonary atresia, the situation can be somewhat more favourable and the opening of the closed pulmonary valve (pulmonary artery valve) by surgery or cardiac catheter intervention allows the small right ventricle to catch up.
1. Aortopulmonary shunt:
The first operation is usually to create a connection between the aorta and the pulmonary artery. For this purpose, a small plastic tube is sewn between the brachial artery and the pulmonary artery. The aortopulmonary shunt replaces the ductus arteriosus, which is then also surgically closed. This ensures the child's oxygen supply, but the patient remains cyanotic (cyanosis). The operation is performed in the first few days of life. In some paediatric heart centres, including ours, the ductus arteriosus can be fitted with a vascular support (stent) as an alternative to the aortopulmonary shunt. This is done in a cardiac catheter intervention, so that surgery is not initially necessary. In combination with an opening of the pulmonary valve, also in the cardiac catheter laboratory (radiofrequency perforation) Link, the situation may develop so favourably that the right ventricle takes over more and more of its intended work and no further operations are necessary.
2. Glenn operation:
If the conditions are not so favourable, the large vein of the upper half of the body (superior vena cava) is connected to the pulmonary artery (Glenn operation) at the age of 4-6 months and the aortopulmonary shunt or stented duct is surgically closed at the same time.
3. Total cavapulmonary anastomosis (TCPC):
As with hypoplastic left heart syndrome, in all those patients in whom the right ventricle remains too small at the age of 3 years (2-4 years), the large vein of the lower half of the body (inferior vena cava) is also connected to the pulmonary artery. For this purpose, a plastic tube is sewn between the two blood vessels. This idea of supplying venous blood to the lungs was first invented by the Frenchman "Francis Fontan" in the 1980s, and the circulation that is achieved with it is also known as the Fontan circulation. From this point onwards, patients no longer have cyanosis (cyanosis).