Tetralogy of Fallot (TOF) is the most common cyanotic heart defect (heart defect with cyanosis) and comprises the following four changes (in Greek tetra means four) in the heart:
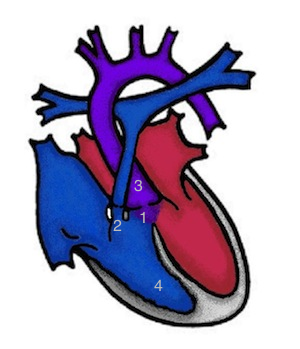
1 – A large ventricular septal defect (VSD) = hole in the ventricular septum
in the ventricular septum
2 – A narrowing (stenosis) of the outflow tract of the right ventricle
ventricle below the pulmonary artery
(infundibular stenosis)-2a and/or a narrowing of the pulmonary
pulmonary artery valve (valvular stenosis)
3 – The aorta (main artery of the body) is enlarged and
"rides" over the ventricular septal defect
(overriding aorta).
4 – A thickening of the musculature of the right ventricle
(right ventricular hypertrophy)
In up to 1/3 of patients, a so-called right aortic arch is found.
What impact does Fallot's tetralogy have?
The narrower the outflow tract of the right ventricle, the more blue the child will be, as more deoxygenated blood flows from the right ventricle directly into the aorta (right-to-left shunt). The narrowness of the right outflow tract generally increases in the first few months of life. This cyanosis can best be seen on the lips.
Symptoms
In particularly severely affected babies, cyanosis can intensify acutely. Such "cyanosis attacks" can be life-threatening.
In the most severe form of tetralogy of Fallot, the pulmonary artery valve (pulmonary atresia) is missing, so that no blood flows from the right ventricle into the lungs. In these babies, the drug prostaglandin must be administered immediately after birth to keep the ductus arteriosus (the vessel that connects the aorta to the pulmonary artery and normally closes in the first few days of life) open so that blood can flow into the lungs.
How is Fallot's tetralogy treated?
An aortopulmonary shunt as an initial procedure is rarely necessary nowadays. A plastic tube (shunt) is usually sutured between the brachial artery and the pulmonary artery. Alternatively, balloon dilatation of the pulmonary valve can be used to increase pulmonary blood flow and thus improve cyanosis. As a substitute for shunt surgery, an attempt can be made to keep the duct open with a stent.
Corrective surgery is usually performed between the third and sixth month of life. This involves removing tissue that is narrowing the outlet from the right ventricle. Patches made of autologous or synthetic material are used to close the ventricular septal defect and widen the outflow tract of the right ventricle and the pulmonary artery. If a shunt operation was previously performed, the shunt is removed. If no pulmonary valve is present, the surgeon implants a biological valve from another person (homograft) or from an animal (xenograft). The most commonly used valve in small children is taken from the jugular vein of the calf (ContegraTM).
Particular attention must be paid to the pulmonary artery valve during follow-up checks, as it often no longer closes completely tightly after the surgical expansion. After a few years, it may be necessary to replace the valve. In a large number of patients, this can be carried out without further surgery by implanting a heart valve in the cardiac catheterisation laboratory (Melody valve).
Patients with tetralogy of Fallot require lifelong monitoring, as the extensive corrective surgery leaves scars in the heart. These can still cause cardiac arrhythmias decades later.
However, the prognosis of patients with tetralogy of Fallot has improved dramatically. The earlier timing of surgery, refined surgical techniques and the possibilities of cardiac catheterisation have contributed to this.