by Anja Dobrijevic
Photos by: Anja Dobrijevic
Over 40% of people worldwide suffer from obesity. This is not simply our greed and laziness. It is a result of an out-of-control modern lifestyle. The food and beverage industry promotes snacks, soft drinks, and instant meals for our convenience. By this advertising, we are convinced that sweet, fat-filled foods are what we deserve as a treat or a reward. This together with our busy lifestyle makes it difficult to resist and that is partly why obesity rates are increasing. Obesity is a major health problem as it leads to various other diseases such as high blood pressure, heart-related problems, mental illnesses such as clinical depression and anxiety, many different cancers, liver disorders, and many more. To store the energy of this food we have an organ called adipose tissue, or just fat.
Adipose tissue is made up of stromal vascular cells and fat cells called adipocytes, which are responsible for fat (lipid) storage. However, adipocytes cannot store an unlimited amount of lipids. In obesity when this limit is reached, it causes ectopic lipid deposition, which then leads to chronic inflammation and cell death. In this case, lipids are stored in other organs which are not meant for lipid storage such as the liver, and this leads to the development of fatty liver disease. We are interested in this crosstalk between adipose tissue and liver and in special sort of immune cells called macrophages. Macrophages are believed to be important players in these processes because of their function as inflammation mediators, and as such, they may be targets for future treatments. In this project, we are investigating the function of different receptors expressed by macrophages, which can take up different kinds of lipids as well as dead or dying cells. During obesity, the abundance of lipids increases and macrophages change their affinity to take up different lipids by expressing more of these receptors.
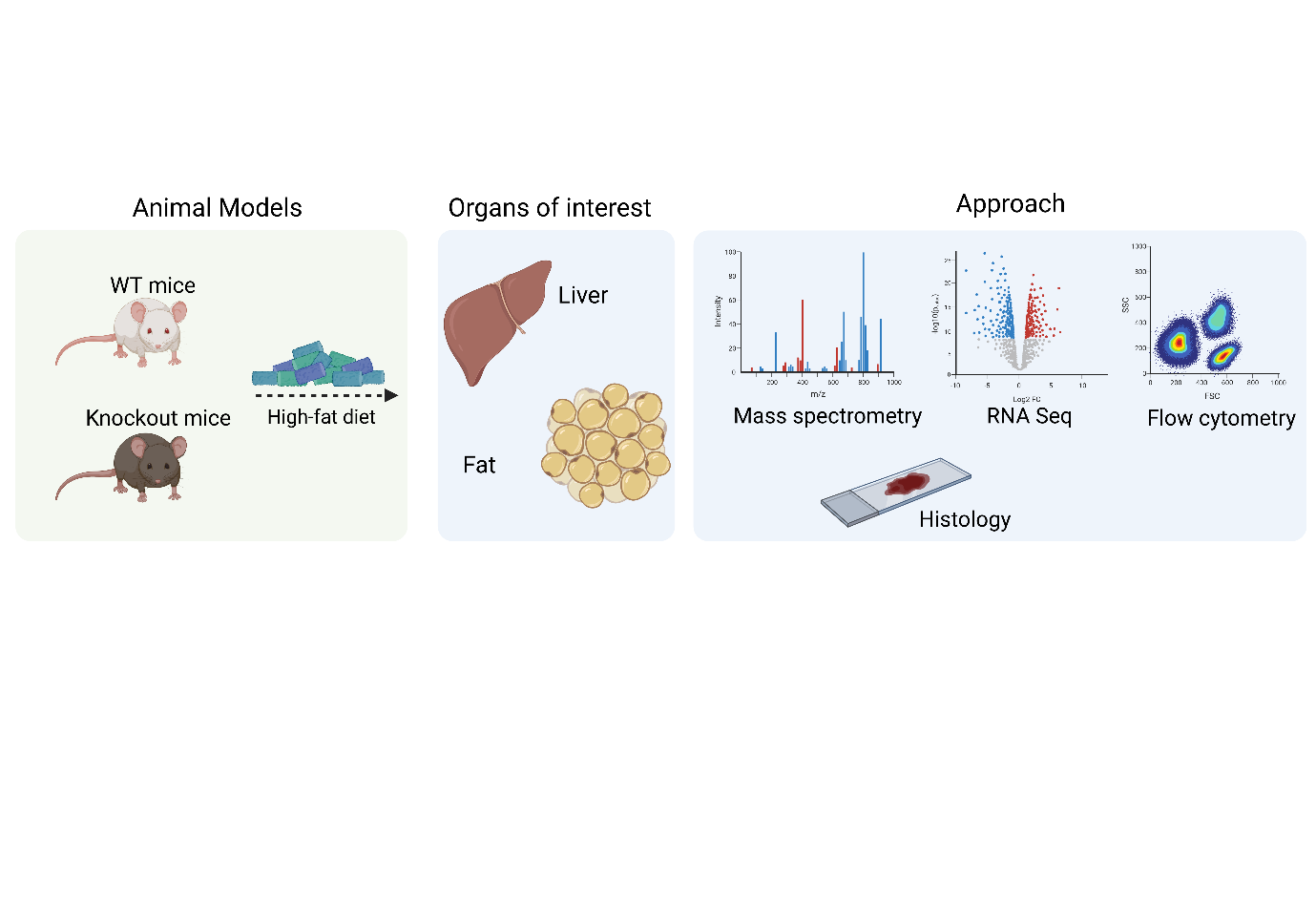
To investigate the function of these receptors, we put mice lacking these receptors on a high-fat diet to make them fat and then compare the phenotype of these mice to wild-type mice having those receptors. We then perform different approaches including flow cytometry to examine the abundance of different cell populations, mass spectrometry to check the alternations in lipids and metabolites, RNA sequencing to analyze gene expression, and different histological staining. These experimental approaches are performed in different organs, especially the liver and adipose tissue. The scheme of the experimental setup can be seen below.
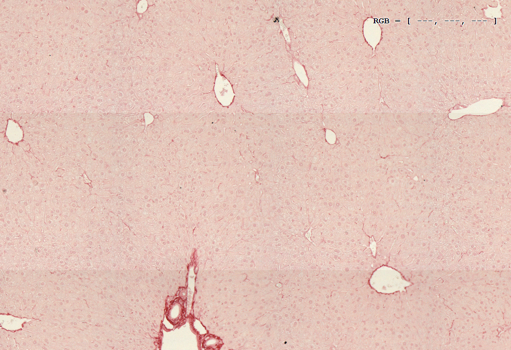
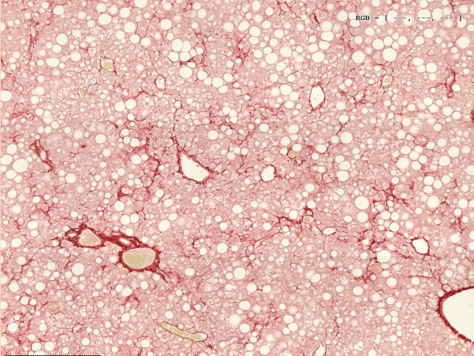
Sometimes humans having obesity and fatty liver develop fibrosis, which is a wound healing process that has gone awry and results in detrimental scarring of organs and their dysfunction. To measure fibrosis levels in our mice, we perform Sirius red staining of liver sections depicted in the picture below. On the left-hand side is a non-fibrotic liver from lean mice and on the right side is a fibrotic liver of obese mice.
As already mentioned, obesity leads to cell death, which is another aspect of this project.
The process of taking up the dying of dead cells and therefore maintaining tissue homeostasis is called efferocytosis. Our favorite cells macrophages eat these dying cells through receptors we are investigating. To investigate the capability of our knockout macrophages to eat, we isolate primary macrophages from mice, feed them with dying cells, and then measure their efferocytotic capacity by flow cytometry. If you are more interested in what our lab is doing, please check out the website: Sharif, Omar | MedUni Wien